Flow & Floor: How Your Menstrual Cycle Impacts Pelvic Floor Function (and dysfunction)
Mood swings, low energy, digestive changes, painful sex, bladder issues—sound familiar at certain points in your cycle? These shifts aren’t random. Your hormones play a powerful role in how your pelvic floor functions throughout the month. Let’s break down the four hormones involved, how each menstrual phase affects the pelvic floor, and how pelvic floor physical therapy can help you feel more supported and in control.
Why Hormones Matter for Pelvic Floor Function:
Women have two major reproductive hormones: estrogen and progesterone and they are released by the ovaries. These two important hormones work together to regulate the menstrual cycle, support pregnancy, and influence tissues beyond the reproductive system (pelvic floor, bladder, brain, nerves, bones, and skin)
- Think of estrogen as the builder and stabilizer hormone. It helps support your bones, skin and connective tissue, including your vaginal wall and pelvic floor tissue.
- Now, think of progesterone as the calmer & protector hormone. Its main role is to prepare the body for pregnancy while also affecting our “rest and digest” or parasympathetic nervous system.
Women have two other very important hormones that are not released by the ovaries but by a small gland at the base of the brain called the anterior pituitary gland. Those are called Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). These hormones are key in managing the estrogen and progesterone levels. Without LH, ovulation wouldn’t happen, and progesterone levels would not rise to prepare for pregnancy. Without FSH, follicles (the fluid-filled sacs that contain eggs) would not mature, estrogen would not rise, and ovulation would not occur. Needless to say, hormonal regulation is so important for menstrual function!
Now that we've established the role of the primary hormones of the menstrual cycle, let's dive into where these levels fluctuate throughout the menstrual cycle and how the pelvic floor responds to those changes. Understanding these patterns can make exercise, intimacy, and self-care so much easier and allow you to work with your body.
The Menstrual Cycle and The Pelvic Floor Muscles
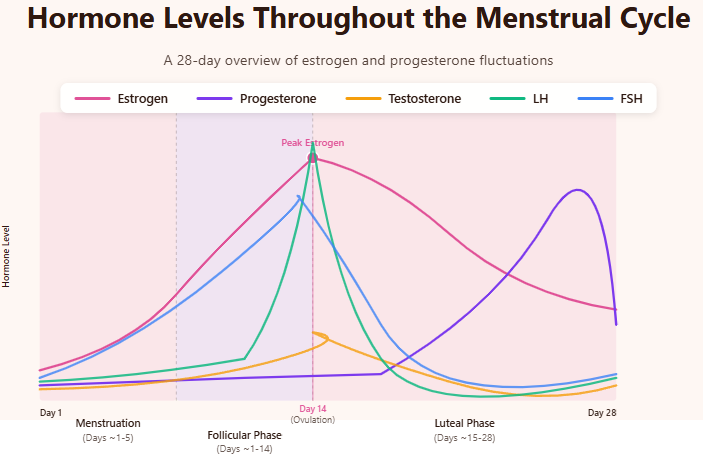
The menstrual cycle is a repeating series of hormonal and physical changes that prepare the body for the possibility of pregnancy. It typically lasts about 28 days, though cycles anywhere from 21 to 35 days can be normal. This cycle is controlled by a very complex interaction between the brain, hormones, ovaries, and uterus.
Menstrual Phase: (days ~1-5)
What is happening:
Your Uterine lining sheds because pregnancy did not occur. This is also known as your period.
Hormones:
Estrogen & progesterone are at their LOWEST
What does this mean for your pelvic floor:
- Muscles may feel heavier, achier, or more sensitive.
- Cramps from the uterus can cause pelvic floor muscle guarding.
- Some women experience increased back or pelvic tension.
- If you have underlying pelvic floor hypertonicity (increased activity in the muscles at rest), you may experience pelvic pain with use of menstrual products like diva cup, discs, and tampons.
- Increased tension in the pelvic floor muscles can intensify period cramp pain and discomfort.
What helps:
- Gentle stretching, mobility work, and diaphragmatic breathing
- Heat therapy
- Light walking or yoga
- Reducing high-impact or max-load strength training if your body feels tense
This a good time to focus on pelvic floor relaxation rather than hard contractions
Follicular Phase: (days ~1-14)
What is happening:
Body begins preparing for ovulation, by thickening up the lining in the uterus (endometrium)
Hormones:
- Estrogen rises; progesterone remains low
- FSH rises, stimulating several follicles in the ovary to grow
What does this mean for your pelvic floor:
- Pelvic floor muscles often feel stronger, more coordinated, and more responsive
- Tissue elasticity improves, meaning clearer skin, healthier vaginal tissue, softer muscles (this is a good thing!), and more collagen production overall
- Pain sensitivity tends to be lower
This is your pelvic floor’s “sweet spot.”
Strength training, advanced pelvic floor activation, and more intense exercise often feel easier here.
Ovulation: (Mid-cycle, around Day 14)
What is happening:
The ovary releases the mature egg and it's the most fertile time
Hormones:
- Estrogen and LH both peak (HIGHEST)
- Rise in FSH
- Small testosterone rise
What does this mean for your pelvic floor:
- Pelvic floor strength and power are often at their best.
- Natural lubrication increases due to high estrogen—helping with intimacy and comfort.
- Some women feel a brief pelvic twinge, which can tighten the pelvic floor temporarily.
What helps:
- Warm up thoroughly before workouts
- Add coordination work: core engagement, breath syncing, dynamic pelvic floor activation
Luteal Phase: (Days ~15-28)
What is happening:
After ovulation, the body prepares for a possible pregnancy by making the lining thick, vascular, and stable.
Hormones:
Progesterone RISES, then drops pre-period.
What does this mean for your pelvic floor:
- Higher progesterone can increase bloating and fluid retention → heaviness in the pelvis.
- Pelvic floor muscles may feel more fatigued or less coordinated.
- Late luteal phase (PMS window) often brings heightened pain sensitivity.
- Some women experience more bladder urgency or frequency
What helps:
- Moderate-intensity exercise
- Stress-reducing breathwork (progesterone shifts can impact mood and anxiety)
- Gentle pelvic floor strengthening
- Focusing on relaxation techniques as your period approaches
Common Pelvic Floor Symptoms That Change with Your Cycle
Women often report fluctuations such as:
- Pelvic pressure or heaviness
- Increased leaking or urgency near their period
- Painful intercourse around menstruation
- Pelvic floor tension during PMS
- More difficulty coordinating pelvic floor contractions late in the cycle
These symptoms are normal patterns, but they shouldn’t be debilitating. Pelvic PT can help regulate and reduce them!
When to See a Pelvic Floor Physical Therapist
If your cycle comes with:
- pelvic pain
- painful intercourse
- bladder leaking
- increased frequency of urination or urgency
- recurrent heaviness or prolapse symptoms
- constipation or straining
- or unpredictable pelvic floor tension
…these are signs your pelvic floor muscles may be overworking or under-coordinating. You don’t have to navigate that alone—pelvic PT can help restore comfort, confidence, and healthy function.
References:
References:
Junge, K., Mann, U., et al. (2019). The influence of hormones on pelvic floor muscle activity. International Urogynecology Journal, 30, 245–252. (Direct evaluation of pelvic floor muscle behavior across hormonal states.)
Kodete CS, Thuraka B, Pasupuleti V, Malisetty S. Hormonal Influences on Skeletal Muscle Function in Women across Life Stages: A Systematic Review. Muscles. 2024 Aug 21;3(3):271-286. doi: 10.3390/muscles3030024. PMID: 40757596; PMCID: PMC12225299. Link: https://pmc.ncbi.nlm.nih.gov/articles/PMC12225299/
Hines, T. J., et al. (2019). Hormonal influences on pain sensitivity across the menstrual cycle. Pain, 160(9), 2051–2060.
McNulty, K. L., Elliott-Sale, K. J., Dolan, E., et al. (2020). The effects of menstrual cycle phase on exercise performance in eumenorrheic women: A systematic review and meta-analysis. Sports Medicine, 50(10), 1813–1827.https://pubmed.ncbi.nlm.nih.gov/32661839/
Sung, E., Han, A., Hinrichs, T., Vorgerd, M., Manchado, L., & Platen, P. (2014). Effects of follicular vs. luteal phase–based strength training in young women. International Journal of Sports Medicine, 35(7), 591–597.https://pubmed.ncbi.nlm.nih.gov/25485203/



