Tailbone pain? It could be your pelvic floor
What is Tailbone Pain (Coccydynia)?
If you’ve ever bruised your tailbone, you already know: it’s no joke. Sitting hurts, standing can feel stiff, and even using the bathroom isn’t always easy. That annoying ache at the bottom of your spine? It’s called coccydynia (pronounced "cock-sid-IN-ee-uh"), and while it sounds fancy, it just means tailbone pain. What a lot of people (and yes, even some doctors) don’t realize is that your pelvic floor muscles might be part of the problem or even the main reason your tailbone is hurting in the first place.
Understanding the Pelvic Floor and Its Role
Your pelvic floor is a group of muscles that sit at the bottom of your pelvis like a hammock. These muscles help support your bladder, bowel, and uterus (if you have one), and they’re involved in things like posture, peeing, pooping, and sex. Some of these muscles actually attach directly to your tailbone (also called the coccyx). So, if your pelvic floor muscles get too tight, tense, or don’t coordinate properly, they can pull on your tailbone and cause pain. On the flip side, if you injure your tailbone (like from a fall or tough labor) your pelvic floor muscles may tighten up to protect you, which can make things worse.
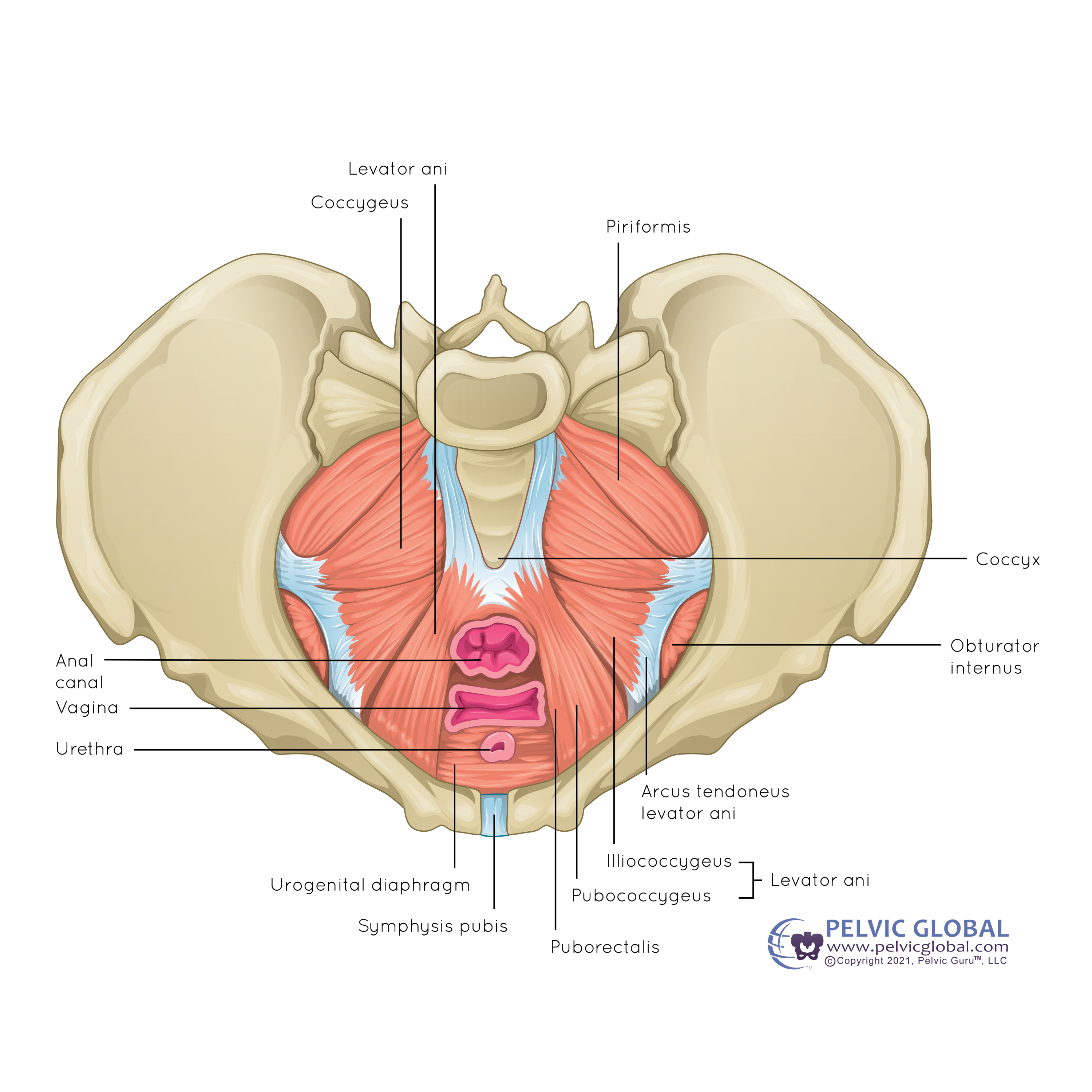
A particularly important group of muscles here is called the levator ani. The levator ani is made up of three parts: the pubococcygeus, the puborectalis, and the iliococcygeus muscles. These muscles form most of the pelvic floor “hammock.” The pubococcygeus actually connects directly to the coccyx, meaning any tightness or spasms here can directly tug on your tailbone. Problems with the levator ani muscles such as muscle spasms or weakness, are common in people with both pelvic pain and tailbone pain. That’s why targeting these muscles in physical therapy can be so helpful. In daily life, these muscles engage whenever you sneeze, laugh, lift something heavy, or even just sit upright, which is why keeping them healthy matters.
Common Causes of Tailbone Pain
Tailbone pain can be caused by a few common culprits:
- Falling on your bottom (on ice, stairs, or during sports)
- Sitting for too long (especially on hard surfaces)
- Childbirth (especially a long or difficult labor)
- Repetitive movement like biking or rowing
- Poor posture or weak core muscles
- Chronic constipation and straining
- Extra weight putting pressure on the tailbone
It’s also more common in women, possibly because of the way the pelvis is shaped and how the tailbone moves during childbirth.
What Research Shows About Pelvic Floor and Tailbone Pain
Research backs up the pelvic floor connection. A 2022 study found that nearly half of women who sought pelvic floor physical therapy for chronic pelvic pain also had tailbone pain. These women were more likely to have muscle spasms in their pelvic floor, issues with constipation, and difficulty coordinating bowel movements. That tells us that if you're only treating your tailbone and ignoring your pelvic floor, you might be missing a big part of the problem.
How to Help Your Tailbone and Pelvic Floor
Good news: you don’t have to suffer in silence or live on donut cushions forever. There are plenty of things you can do to feel better.
Here’s what works from evidence based research:
- Pelvic Floor Physical Therapy
A specially trained therapist can check if your muscles are tight, weak, or not coordinating well. They may work on releasing tight areas (sometimes internally through the vagina or rectum), and teach you how to relax those muscles and use them more efficiently. This can help not only your tailbone, but also with constipation, posture, and even discomfort during sex. Therapy often includes exercises to strengthen weak muscles and relax tight ones, retraining how you use your pelvic floor during everyday movements like sitting, walking, and bathroom use. - Coccyx Mobilization
Sometimes your tailbone can get stuck in a tilted or rotated position. A trained physical therapist can gently help restore its natural movement, often from inside the rectum. This might sound unusual, but it’s a well-documented and often effective treatment for chronic tailbone pain. - Stretching and Strengthening
Tight hips and weak glutes or core muscles can all affect your pelvic balance. Targeting muscles like your piriformis, hip flexors, glutes, and abdominals can ease pressure on your tailbone and help your whole pelvis move better. Gentle yoga or specific stretches prescribed by a therapist can help loosen tight muscles that pull on your pelvic floor and tailbone. - KT Tape (Kinesiology Taping)
When applied to the lower back or pelvis, this stretchy tape can help support the area, reduce muscle tension, and improve posture. Research shows combining tape with physical therapy may lead to better results. - Toilet Tips: Try a Footstool
Straining on the toilet is a major stressor on both the pelvic floor and tailbone. Using a small footstool (like the Squatty Potty) helps position your body in a more natural squat, making bowel movements easier and less stressful on your pelvic floor. This position straightens the rectum and can reduce the pressure and strain that might worsen tailbone pain. - Cushions That Actually Help
If sitting is painful, special cushions designed to offload pressure from the tailbone can help. U-shaped cushions take pressure off the coccyx, donut cushions create space in the center, and wedge cushions help tilt your pelvis slightly forward for better posture. Memory foam cushions or gel pads can also provide comfort for longer sitting periods, like at work or during travel. Trying different cushions can help you find the best fit for your body.
Other simple lifestyle changes can help too: sit with better posture, avoid slumping, change positions often, stay active, eat plenty of fiber, drink enough water, and avoid pushing or straining during bowel movements.
When to See a Pelvic Floor Therapist
When should you consider seeing a pelvic floor therapist? If your tailbone pain has lasted more than a few weeks, or if you’re also having pain while sitting, constipation, painful sex, or any kind of pelvic, hip, or lower back discomfort, it’s time. These symptoms are often connected, and a physical therapist can help get to the root of what’s going on.
You Don’t Have to Live with Tailbone Pain
The bottom line? Tailbone pain and pelvic floor issues often go hand in hand. The good news is that they’re both highly treatable, especially with the right kind of help. Whether your pain started from a fall, a baby, a long bike ride, or just too much time at a desk, there are simple, research-backed ways to start feeling better. With the right stretches, strengthening, muscle retraining, and expert care, you can sit comfortably again and feel like yourself.
Resources:
Garg, B., & Ahuja, K. (2021). Coccydynia—A comprehensive review on etiology, radiological features and management options. Journal of Clinical Orthopaedics and Trauma, 12(1), 123–129. https://doi.org/10.1016/j.jcot.2020.09.025
Neville, C. E., Carrubba, A. R., Li, Z., Ma, Y., & Chen, A. H. (2022). Association of coccygodynia with pelvic floor symptoms in women with pelvic pain. PM&R: The Journal of Injury, Function, and Rehabilitation, 14(11), 1351–1359. https://doi.org/10.1002/pmrj.12706
Mosaad, E. H., Mohamed, A. Y., Fawzy, A. A., & Mohamed, M. H. (2023). The effect of adding kinesiotaping versus pelvic floor exercise to conventional therapy in the management of post-colonoscopy coccydynia: a single-blind randomized controlled trial. African health sciences, 23(1), 575–583. https://doi.org/10.4314/ahs.v23i1.60
Sidiq, M., Ravichandran, H., Janakiraman, B., Chahal, A., Rai, R. H., Alotaibi, A. H., Alotaibi, A. H., Alotaibi, A. S., Ibrahim, A. A., Alharbi, E. A., Kashoo, F. Z., & Vats, H. (2025). Effectiveness of physical therapy interventions for coccydynia: a systematic review with a narrative synthesis. Archives of physiotherapy, 15, 77–89. https://doi.org/10.33393/aop.2025.3233
Maigne, J. Y., & Chatellier, G. (2001). Comparison of three manual coccydynia treatments: a pilot study. Spine, 26(20), E479–E484. https://doi.org/10.1097/00007632-200110150-00024
Kara, D., Pulatkan, A., Ucan, V., Orujov, S., & Elmadag, M. (2023). Traumatic coccydynia patients benefit from coccygectomy more than patients undergoing coccygectomy for non-traumatic causes. Journal of orthopaedic surgery and research, 18(1), 802. https://doi.org/10.1186/s13018-023-04098-5
Lewis, G. K., Chen, A. H., Craver, E. C., Crook, J. E., & Carrubba, A. R. (2023). Trigger point injections followed by immediate myofascial release in the treatment of pelvic floor tension myalgia. Archives of gynecology and obstetrics, 307(4), 1027–1035. https://doi.org/10.1007/s00404-022-06880-y



